Can Testosterone Therapy Reduce the Risk of Dementia?
Last Updated: November 2025
Testosterone is often thought of as the “sex hormone,” but it’s far more than that. It’s also a neuroprotective hormone — critical for brain energy, mood, and memory.
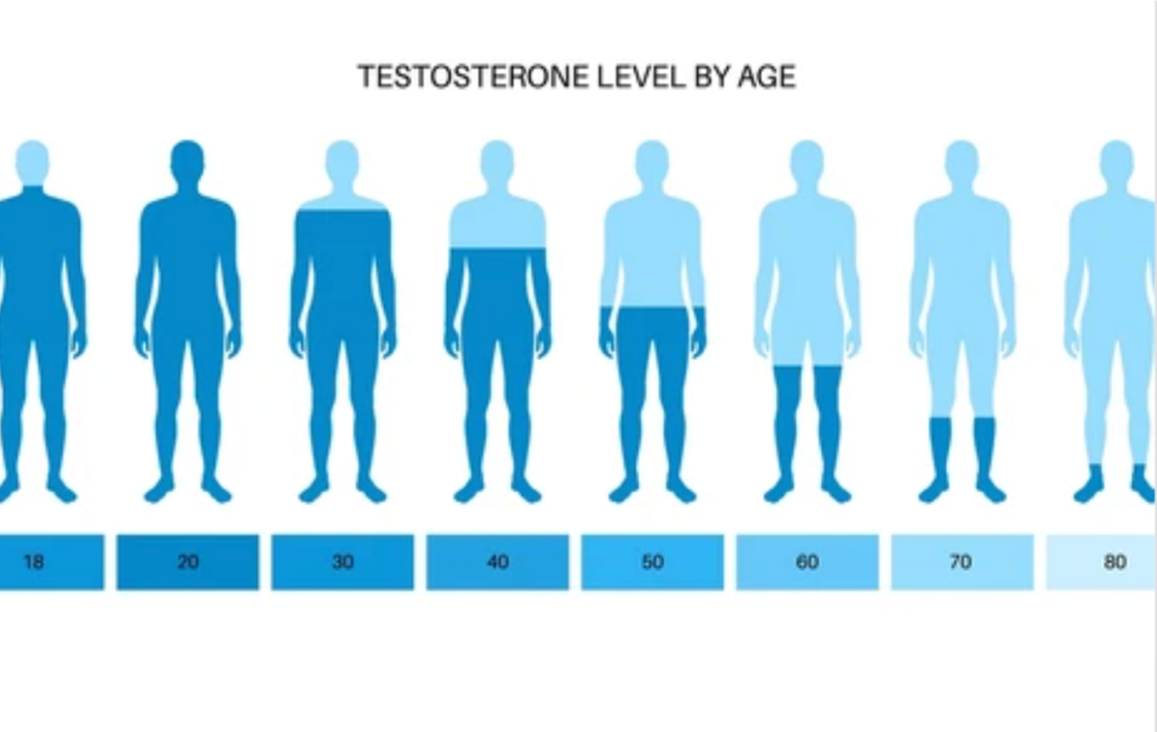
As men age, testosterone levels gradually decline. This change is natural, but when levels fall too low, the effects go beyond libido or muscle tone.
Research now links low testosterone to depression, brain fog, and even higher dementia risk.
At HealthSpan Internal Medicine in Boulder, CO, we approach testosterone therapy not as a cosmetic or performance choice, but as a metabolic and cognitive intervention — a way to support vascular, mitochondrial, and neurological longevity.
HealthSpan Insight
Low testosterone increases the risk of memory loss and cognitive decline.
Testosterone supports neuron growth, oxygen flow, and neurotransmitter balance.
Safe, evidence-based replacement can enhance vitality and brain function — when done correctly.
1. Testosterone’s Role in Brain Health
Testosterone affects far more than sexual function.
The brain is rich in androgen receptors, especially in regions tied to focus, motivation, and memory — such as the hippocampus and prefrontal cortex.
Testosterone helps the brain by:
Enhancing blood flow: Increases nitric oxide, improving oxygen and nutrient delivery.
Supporting synaptic plasticity: Promotes growth of new neural connections.
Reducing inflammation: Lowers microglial activation and cytokines linked to neurodegeneration.
Protecting mitochondria: Boosts energy metabolism and antioxidant defense.
Balancing neurotransmitters: Supports dopamine, serotonin, and acetylcholine — key for motivation, mood, and cognition.
When testosterone declines, these systems falter — and symptoms like brain fog, apathy, and slower thinking often appear.
2. Low Testosterone and Dementia Risk
Low testosterone (often defined as total T < 350 ng/dL, or free T < 10 ng/dL) is associated with multiple dementia risk factors.
Large population studies have shown:
Men with lower testosterone are more likely to develop Alzheimer’s disease over time.
Low testosterone correlates with smaller hippocampal volume and poorer verbal memory.
Men with low T are more likely to develop metabolic syndrome, insulin resistance, and vascular disease — all key contributors to cognitive decline.
A 2023 study in JAMA Network Open found that men with chronically low testosterone had 30% higher risk of dementia, even after adjusting for age and education.
Why? Because testosterone isn’t just a hormone — it’s a signal of metabolic resilience. When it drops, inflammation rises, nitric oxide falls, and brain energy suffers.
3. The Vascular and Mitochondrial Link
Testosterone has profound effects on blood vessels and mitochondria — the same systems central to both erectile function and brain performance.
Vascular benefits: Testosterone increases nitric oxide synthase activity, improving endothelial function and cerebral perfusion.
Mitochondrial support: It enhances ATP production, reduces oxidative stress, and protects neurons from beta-amyloid toxicity.
When testosterone declines, small-vessel blood flow to the brain decreases, leading to vascular cognitive impairment — often mistaken for early Alzheimer’s.
By restoring testosterone, oxygen delivery improves, inflammation calms, and neurons regain energy.
4. The Inflammatory Cascade of Low Testosterone
Low testosterone triggers a pro-inflammatory environment, raising CRP, IL-6, and TNF-α.
Chronic inflammation accelerates both atherosclerosis and neuroinflammation — the hallmarks of vascular and degenerative dementia.
Testosterone therapy has been shown to lower inflammatory markers and improve insulin sensitivity, breaking that vicious cycle.
5. The Emotional and Cognitive Symptoms of Low Testosterone
Common cognitive and mood symptoms include:
Reduced motivation or drive
Depressive mood or irritability
Fatigue and mental sluggishness
Difficulty concentrating or recalling words
Poor stress tolerance
These changes aren’t “just aging.” They’re often the brain’s response to declining hormonal and mitochondrial support.
6. Can Testosterone Therapy Reverse Cognitive Symptoms?
Early studies suggest that optimizing testosterone can improve memory and mood — particularly in men with mild cognitive impairment or hypogonadism.
A Neurology study (2016) found that six months of testosterone therapy improved verbal memory and spatial ability in older men with low T.
Other trials show improved processing speed, attention, and mood after restoring testosterone to physiological range.
Functional MRI studies show better blood flow and oxygenation in brain regions linked to memory after therapy.
While testosterone therapy is not a “cure” for dementia, it can slow progression, especially when paired with exercise, nutrition, and sleep optimization.
7. How Testosterone Therapy Works (and What to Expect)
There are several safe, evidence-based options for restoring testosterone:
Topical gels or creams: Easy to titrate, daily use.
Injections (cypionate, enanthate): Usually weekly or biweekly dosing.
Pellets: Longer-acting forms for convenience.
The goal is physiologic restoration, not “bodybuilder levels.”
At HealthSpan, we aim for total testosterone between 600–900 ng/dL and free T in the upper-normal range.
Monitoring is key:
We track estradiol, hematocrit, PSA, liver function, and lipid profile to ensure therapy remains safe and balanced.
8. Is Testosterone Therapy Safe for the Prostate and Heart?
Contrary to old myths, current evidence shows that testosterone therapy does not increase prostate cancer risk when properly monitored.
A 2021 meta-analysis of over 30 studies found no increase in prostate cancer incidence among men receiving testosterone therapy.
In fact, men with low testosterone have higher rates of aggressive prostate cancer, suggesting low T may be a risk marker, not a cause.
Similarly, cardiovascular safety data now show that testosterone replacement reduces all-cause mortality in men with metabolic syndrome or hypogonadism — likely due to improved endothelial and insulin function.
9. Natural Strategies to Boost Testosterone and Brain Health
For men who prefer a natural approach — or as an adjunct to therapy — foundational habits make a big difference:
Strength training: Lifts both testosterone and brain-derived neurotrophic factor (BDNF).
Adequate protein and healthy fats: Zinc, vitamin D, and omega-3s are essential for hormone synthesis.
Reduce stress and sleep apnea: Cortisol and poor sleep both suppress testosterone and impair brain detox.
Healthy body composition: Even modest fat loss can increase free testosterone and improve cognition.
10. The Bottom Line
Low testosterone isn’t just about libido — it’s a metabolic and neurological signal that your body and brain are under strain.
Restoring optimal testosterone supports vascular health, mitochondrial energy, and cognitive resilience.
When done safely and monitored carefully, testosterone therapy can help men stay sharp, energized, and connected — physically and mentally — as they age.
At HealthSpan Internal Medicine in Boulder, CO, we combine functional testing, hormone optimization, and brain-centered care to help men preserve both vitality and cognition across their lifespan.
Testosterone is only part of the story—your brain deserves a full picture.
Meet with Dr. Knape to integrate hormones, genomics, vascular markers, and cognition into a comprehensive plan for long-term brain health.
Reserve your BrainSpan Discovery Call.
Sources
Testosterone, Cognitive Decline & Dementia in Aging Men, Yeap BB et al., 2022 Review — PMC
Sex Hormones, Brain Aging & Neurodegeneration Mechanisms, Wiley Review, 2024
Testosterone Levels, Vascular Risk & White Matter Changes, UK Biobank Cohort, 2022
Medically reviewed by
Dr. Jessica Knape, MD, MA Board Certified in Internal Medicine and Integrative and Holistic Medicine
Healthspan Internal Medicine — serving patients in Boulder, CO
Book a Discovery Call | About Dr. Knape
This content is for educational purposes and does not replace personalized medical advice.