What Are the Top New Treatments for Alzheimer’s Disease?
The field of Alzheimer’s disease (AD) treatment is changing faster than ever. After decades of frustration, researchers are finally identifying therapies that do more than just manage symptoms—they may actually change the course of the disease.
At HealthSpan Internal Medicine in Boulder, CO, we keep our patients informed on both evidence-based treatments and emerging options available through clinical trials or compassionate use. Below is an overview of the most promising therapies—from advanced biologics to repurposed medications and brain-supportive supplements.
The HealthSpan Summary
FDA-approved drugs still focus mainly on amyloid removal and symptom relief.
New trials are targeting inflammation, metabolism, tau protein, mitochondria, and neuroprotection.
Repurposed drugs like GLP-1 agonists (semaglutide, liraglutide) and metformin show strong potential.
Nutrient therapies like B vitamins, omega-3s, and Souvenaid® support brain structure and slow decline in early stages.
Experimental drugs like TB006 (anti-galectin-3) aim to stop the root inflammatory processes that drive dementia.
1. The Next Generation of Anti-Amyloid Drugs
Amyloid-beta plaques are one hallmark of Alzheimer’s disease. The newest treatments aim to remove toxic amyloid earlier and more safely than older drugs.
Remternetug (Eli Lilly) – A next-generation monoclonal antibody now in late-phase trials. It may allow subcutaneous (under-the-skin) dosing instead of IV infusions and shows strong amyloid clearance in early studies.
ALZ-801 (valiltramiprosate, Alzheon) – An oral medication designed to block amyloid oligomers (the smaller, more toxic forms of amyloid). It appears most effective in people with the APOE4/4 genotype. This could become the first genotype-targeted Alzheimer’s drug if approved.
These drugs work best early, before significant neuron loss has occurred, and require amyloid confirmation by PET or plasma biomarkers.
2. Tau-Targeted Therapies
Tau tangles are the second major brain change in Alzheimer’s.
BIIB080 (Biogen; “tau ASO”) – A first-in-class therapy that uses an antisense oligonucleotide (a short RNA strand) to silence the gene that makes tau protein. It’s showing promise in lowering tau and slowing decline.
This approach could help not only Alzheimer’s but also other “tauopathies” like frontotemporal dementia.
3. Anti-Inflammatory and Multi-Pathway Drugs
Inflammation is now recognized as a key driver of neurodegeneration.
TB006 (TrueBinding) – A monoclonal antibody that blocks galectin-3, a protein that triggers brain inflammation and worsens amyloid and tau buildup. Early human trials show cognitive stabilization in some patients. It’s currently in Phase 2 and available through compassionate use at select centers.
Buntanetap (Annovis Bio) – A small molecule designed to reduce several neurotoxic proteins and oxidative stress at once. Early studies show functional improvement and reduced inflammatory markers.
Both of these drugs reflect a new strategy: targeting the root inflammation, not just the symptoms.
4. Metabolic Therapies: Rethinking the “Type 3 Diabetes” of the Brain
Metabolic dysfunction—especially insulin resistance—is one of the strongest, modifiable risk factors for dementia.
Semaglutide (Ozempic®, Wegovy®) – A GLP-1 receptor agonist originally developed for diabetes and weight loss. Large clinical trials (EVOKE and EVOKE+) are testing whether it can slow cognitive decline by improving brain insulin sensitivity and reducing inflammation.
Liraglutide (Victoza®) – An older GLP-1 drug with small studies showing less brain shrinkage and subtle cognitive benefits.
Metformin – The widely used diabetes medication appears to lower dementia risk in population studies. Current trials are exploring whether it improves mitochondrial efficiency and brain metabolism directly.
At HealthSpan, we often focus on metabolic optimization—balancing glucose, insulin, and lipids—as a cornerstone of cognitive longevity.
5. Mitochondrial and Energy-Repair Strategies
Brain cells are energy-intensive. When mitochondria slow down, neurons can’t keep up with the demands of learning and memory.
Nicotinamide (vitamin B3) and Nicotinamide Riboside (NR) support NAD+ production, a key molecule for cellular energy and DNA repair. While early studies show safety, results are mixed on measurable cognitive benefit.
Combining NAD+ precursors with exercise, sleep optimization, and oxygen-based therapies may offer additive benefit by recharging mitochondrial health.
6. Neuro-Nutrient and “Medical Food” Support
Souvenaid® (Fortasyn Connect) – A medical food containing a blend of omega-3 fatty acids, choline, B vitamins, antioxidants, and uridine. In multiple European studies, Souvenaid slowed cognitive and structural brain decline in early Alzheimer’s, though benefits were not seen in moderate-to-severe stages.
B-Vitamins (B6, B12, Folate) – In patients with elevated homocysteine, supplementation reduced brain atrophy rates by 30–50%, especially when combined with omega-3s.
These interventions are safe, accessible, and clinically meaningful as part of prevention or early treatment strategies.
7. Antiviral and Immune-Modulating Approaches
Since viruses such as HSV-1 and EBV have been linked to neuroinflammation, researchers are testing antiviral drugs like valacyclovir in Alzheimer’s patients. Early results have been neutral, but the viral-inflammation connection remains a compelling research area.
Future combination therapies may pair antiviral or immune modulation with metabolic and anti-inflammatory strategies.
8. The Bigger Picture: Combining Modalities
The era of “single-target” Alzheimer’s drugs is ending. The most promising future involves layering treatments:
Amyloid or tau reduction (e.g., ALZ-801, BIIB080)
Inflammation control (TB006, lifestyle, gut-brain modulation)
Metabolic optimization (GLP-1s, exercise, nutrition)
Mitochondrial repair (NAD+, oxygen therapies, strength training)
Cognitive support (sleep, light therapy, social connection)
In other words, the same systems that keep your body healthy—energy, oxygen, and repair—also determine brain resilience.
Where Supplements and Lifestyle Fit In
Even as cutting-edge drugs emerge, lifestyle remains the strongest defense.
At HealthSpan, we focus on:
Metabolic health: Preventing insulin resistance through nutrition and exercise.
Sleep optimization: Deep, restorative sleep clears amyloid via the glymphatic system.
Hormone and oxygen balance: Supporting circulation, thyroid, testosterone, and estrogen levels when clinically appropriate.
Inflammation control: Diet, microbiome support, and, when indicated, peptides or mitochondrial nutrients.
Supplements should support—not replace—comprehensive medical care.
Bottom Line
Today’s Alzheimer’s landscape is the most hopeful it’s ever been.
Amyloid and tau therapies are finally showing measurable clinical benefit.
Inflammation and metabolic approaches are reshaping how we treat and prevent dementia.
Nutrient and lifestyle interventions remain foundational for resilience and long-term protection.
At HealthSpan Internal Medicine, our approach is to evaluate each patient’s biology—genetics, metabolism, oxygenation, sleep, and inflammation—and build a personalized brain longevity plan that integrates both established and emerging therapies.
Curious about the next generation of Alzheimer’s treatments?
Book an appointment with Dr. Knape — she’ll assess whether investigational treatments like TB006 or upcoming tau-targeting therapies might fit your personal risk profile and health goals.
Sources
TB006 — Investigational Galectin-3 Antibody for Alzheimer’s Disease
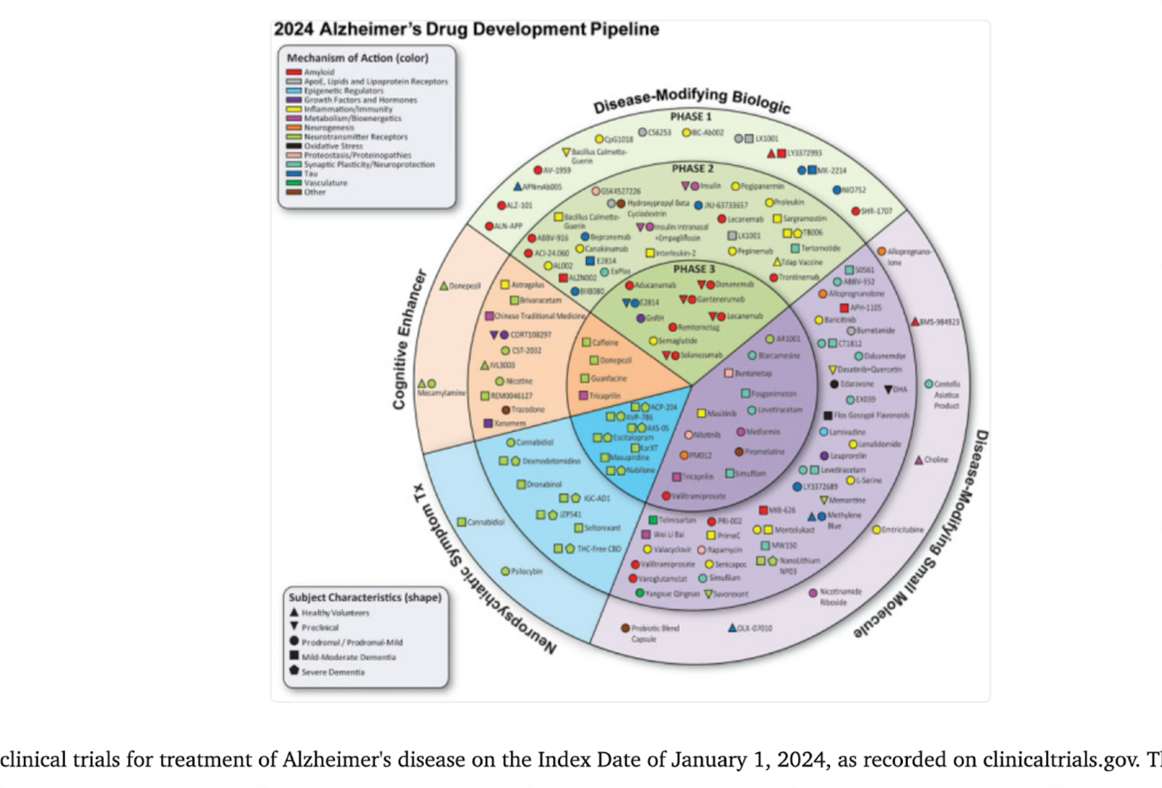
2025 Review of the Alzheimer’s Pipeline — 138 Drugs in 182 Trials
Emerging Tau-Targeted Therapeutics for Tauopathies and Alzheimer’s — 2025 Update
Snapshot of 2025 Alzheimer’s Drug Pipeline — Emphasis on Multi-Target Approaches and Rapid Growth
Medically reviewed by
Dr. Jessica Knape, MD, MA Board Certified in Internal Medicine and Integrative and Holistic Medicine
Healthspan Internal Medicine — serving patients in Boulder, CO
Book a Discovery Call | About Dr. Knape
This content is for educational purposes and does not replace personalized medical advice.