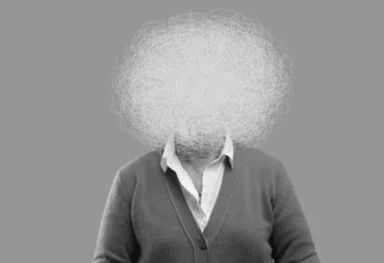
What Is Brain Fog — and When Should I Be Concerned?
Last Updated: November 2025
Almost everyone has experienced “brain fog” — those moments when thinking feels slow, focus slips, or words just won’t come.
But when fog becomes frequent or persistent, it can signal more than simple tiredness.
At HealthSpan Internal Medicine in Boulder, CO, we help patients understand that brain fog is not a diagnosis — it’s a symptom.
And like any signal from the body, it deserves to be decoded, not dismissed.
BrainSpan Insight
Brain fog is a sign that the brain’s energy, oxygen, or communication systems are under stress.
Causes can include inflammation, hormonal imbalance, sleep issues, toxins, or early cognitive decline.
Identifying the root cause early prevents long-term damage and restores mental clarity.
1. What Exactly Is Brain Fog?
“Brain fog” is an informal term for a cluster of symptoms including:
Poor concentration or memory
Slow mental processing
Word-finding difficulty
Mental fatigue
Feeling “spacey,” “out of it,” or easily overwhelmed
Brain fog is essentially neural sluggishness — the brain isn’t producing or using energy efficiently, so thinking feels harder.
This may last hours or days, or become chronic — what we call cognitive fatigue.
2. Why the Brain Gets Foggy
The brain is the body’s most energy-demanding organ, consuming about 20% of total oxygen and glucose.
Anything that disrupts energy production, blood flow, or neurotransmitter balance can dim mental clarity.
Common functional contributors include:
Inflammation: Cytokines interfere with neural signaling.
Mitochondrial dysfunction: Low ATP output reduces cognitive speed.
Hormone imbalance: Low thyroid, progesterone, or testosterone affect focus and mood.
Insulin resistance: Blood-sugar swings cause “energy crashes.”
Toxic burden: Mold, heavy metals, and chemicals inflame brain tissue.
Gut dysbiosis: Inflammatory microbes trigger brain–gut axis stress.
Sleep deprivation: Poor deep sleep prevents synaptic repair.
Often, brain fog reflects whole-body inflammation rather than a brain-localized issue.
3. The Mitochondrial Connection
Mitochondria — the cell’s energy generators — are critical for brain performance.
When they’re overworked or undernourished, neurons can’t fire properly.
This is why conditions that impair mitochondria (viral illness, concussion, toxins, chronic stress) often cause cognitive fatigue.
Therapies that restore mitochondrial function — oxygen therapy, photobiomodulation, methylene blue, CoQ10, and B vitamins — often lift fog dramatically.
4. The Gut–Brain Factor
Your gut produces neurotransmitters like serotonin and GABA, and its microbial balance directly affects mood and focus.
A “leaky gut” allows toxins and inflammatory molecules to reach the brain, activating microglia — the brain’s immune cells.
That’s why people with irritable bowel symptoms often experience fatigue, anxiety, or fogginess.
Healing the gut is often the first step to clearing the mind.
5. Hormones and Brain Clarity
Hormones act as “amplifiers” for brain function.
Thyroid: Regulates brain metabolism and alertness.
Progesterone: Calms the nervous system and supports myelin repair.
Testosterone: Boosts motivation, memory, and processing speed.
Cortisol: Needed for focus, but chronic elevation causes burnout.
Estrogen: Enhances synaptic plasticity and blood flow — especially vital for women in perimenopause.
When these hormones fall out of balance — as they often do with age or stress — fog follows.
6. Inflammation and “Inflamed Brain”
Inflammation in the brain doesn’t cause pain — but it does cause fog.
Triggers include:
Hidden infections (Lyme, Epstein–Barr, long COVID)
Environmental toxins (mold, mycotoxins, pesticides)
Chronic allergies or autoimmunity
Poor diet (refined carbs, seed oils, processed foods)
Inflamed microglia produce cytokines that slow communication between neurons.
That “thick” mental feeling after eating poorly or being exposed to chemicals? That’s neuroinflammation in action.
7. When Brain Fog Is a Red Flag
Occasional fog is normal.
But if it’s persistent, worsening, or accompanied by other symptoms, it’s worth investigating.
Seek professional evaluation if you notice:
Increasing forgetfulness or confusion
Trouble performing familiar tasks
Changes in speech or writing
Depression, apathy, or personality change
Dizziness, imbalance, or blurred vision
Fatigue unrelieved by rest
These may indicate early cognitive impairment, thyroid dysfunction, sleep apnea, or circulatory problems.
At HealthSpan, we perform a comprehensive evaluation that includes:
Hormone and thyroid testing
Inflammatory and oxidative stress markers
Mitochondrial and nutrient status
Gut microbiome and toxin panels
Sleep and oxygen evaluation (if apnea suspected)
8. Root Causes of Persistent Brain Fog
The most common patterns we see include:
A. Blood Sugar Dysregulation
Brain cells rely on steady glucose.
When insulin resistance develops, neurons get less fuel — leading to fatigue, forgetfulness, and irritability.
B. Nutrient Deficiency
Low B12, vitamin D, magnesium, or omega-3s all impair neurotransmission.
These are simple to test and correct.
C. Sleep and Circadian Rhythm
Deep sleep is when the brain’s glymphatic system clears toxins.
Poor sleep means poor detox — leading to next-day fog.
D. Mitochondrial Dysfunction
Low energy output in neurons causes slow processing.
Often seen after infection, concussion, or chronic stress.
E. Infections or Immune Activation
Chronic viruses, Lyme disease, or autoimmunity can cause low-level neuroinflammation.
F. Environmental Exposure
Mold toxins, solvents, or heavy metals can inflame neurons and block energy production.
9. Functional Medicine Approach to Clearing Brain Fog
Rather than masking symptoms, we find and reverse the causes.
Our Brainspan Blueprint™ focuses on restoring three foundations:
Energy, Inflammation, and Communication.
Step 1: Optimize Oxygen and Mitochondria
Photobiomodulation, hyperbaric oxygen, or EWOT
CoQ10, acetyl-L-carnitine, methylene blue (low-dose)
Step 2: Calm Inflammation
Eliminate dietary triggers (sugar, gluten, processed oils)
Use anti-inflammatory nutrients: curcumin, omega-3s, resveratrol
Balance the microbiome with probiotics and prebiotic fiber
Step 3: Support Hormones
Check thyroid, progesterone, testosterone, and cortisol
Use bioidentical hormones or adaptogens as needed
Step 4: Restore Sleep and Glymphatic Flow
Aim for 7–8 hours of restorative sleep
Use breathing exercises or positional therapy for apnea
Gentle exercise and hydration to aid detox
Step 5: Repair the Gut
Heal intestinal permeability
Support digestion and microbial diversity
10. Lifestyle Habits That Keep the Brain Clear
Move every day: Walking, yoga, or resistance training increases brain oxygenation.
Hydrate: Mild dehydration reduces cognitive performance.
Eat colorful plants: Polyphenols feed both the microbiome and mitochondria.
Limit alcohol and sugar: Both impair brain metabolism.
Practice mindfulness or breathwork: Strengthens the vagus nerve and focus.
Protect sleep: Dark, cool room; no screens 90 minutes before bed.
Small habits compound into enormous cognitive benefit.
11. When to Seek Help
If your fog persists for more than a few weeks — or if it interferes with work, relationships, or driving — it’s time for assessment.
Brain fog is often reversible, but early evaluation matters.
Left unchecked, chronic inflammation or metabolic dysfunction can progress toward mild cognitive impairment (MCI) or dementia.
Functional testing can distinguish whether the root is hormonal, inflammatory, mitochondrial, or infectious, allowing precise treatment.
Bottom Line
Brain fog is your body’s way of saying: Something’s off.
It’s rarely “just stress” or “aging.”
With modern functional tools, we can uncover whether the fog stems from poor sleep, hormone shifts, gut imbalance, toxins, or energy deficit — and reverse it.
A clear mind isn’t just luck; it’s a reflection of whole-body balance.
At HealthSpan Internal Medicine in Boulder, CO, we help patients restore mental clarity through targeted testing, precision nutrition, hormone balancing, and mitochondrial support — the foundations of your Brainspan.
If you’ve been told “your labs are fine” but you still feel foggy, tired, or unfocused, it’s time for a deeper look.
Dr. Knape blends clinical experience with advanced biomarkers and functional testing to uncover hidden contributors to brain fog.
👉 Schedule your evaluation.
Sources
“Long COVID brain fog: a neuroinflammation phenomenon?” (PMC article)
“The gut microbiota–brain axis in behaviour and brain disorders” (Nature Reviews Microbiology)
“Gut–Brain Axis: Microbiota, Nervous Systems Interactions” (PMC article)
Medically reviewed by
Dr. Jessica Knape, MD, MA Board Certified in Internal Medicine and Integrative and Holistic Medicine
Healthspan Internal Medicine — serving patients in Boulder, CO
Book a Discovery Call | About Dr. Knape
This content is for educational purposes and does not replace personalized medical advice.